A Truly Epic EHR
What is an EHR, how it puts lives at risk, and a vision for a patient-centric alternative
“Do you know how many clicks it takes for me to order a screening? Six! It takes six clicks to order a simple screening!”
What started as a simple question, “What's wrong with the EHR?” quickly turned into an emotional and educational account of how electronic health record (EHR) software frustrated clinicians on a daily basis.
“Why do they need to ask for confirmation for every single little thing?”
“It’s so hard to use that everyone had to go through mandatory training for this.”
“Do you know the Europeans went on strike because of this software?”
But before diving deeper, let us rewind a little and start with a basic question:
What is an EHR?
During the last visit to my family physician, the clinical assistant riffled through a thick stack of paper folders to find the one containing my medical history. The folder contained barely legible handwritten notes about my previous ailments. Throughout the consultation, my physician squinted at his notes and appended more scribbles.
These pen-and-paper records represent the last vestiges of a healthcare system that is slowly but surely going digital. At the heart of this transition is the EHR, the fundamental building block of the modern digital healthcare stack.
In its basic form, the EHR is simply a digital version of my physician’s handwritten notes. But it also embodies a larger vision: a unified system where all health information—vitals, diagnoses, tests, treatments, medications—is digitized, centralized, and instantly accessible to anyone who needs it.


Back in 2011, A16Z declared that “software is eating the world”. But EHR software had started nibbling at the healthcare industry since the 1970s. Epic Systems, the largest EHR provider, was founded in 1979.
While adoption was relatively slow at the beginning, the HITECH Act in 2009 catalyzed an industry-wide migration to the EHR in the US. The HITECH Act was a carrot-and-stick play—financial incentives for healthcare providers who transitioned to the EHR, and reduced reimbursements for Luddites who insisted on pen-and-paper.

A patient's life scattered across records
The EHR was meant to unify patient data, but in practice this data remains fragmented. Different healthcare providers have their own EHR system, each recording a different facet of a patient’s medical history. Take for example Singapore. Despite our small population and a track record of strong government oversight, data fragmentation remains a challenge.
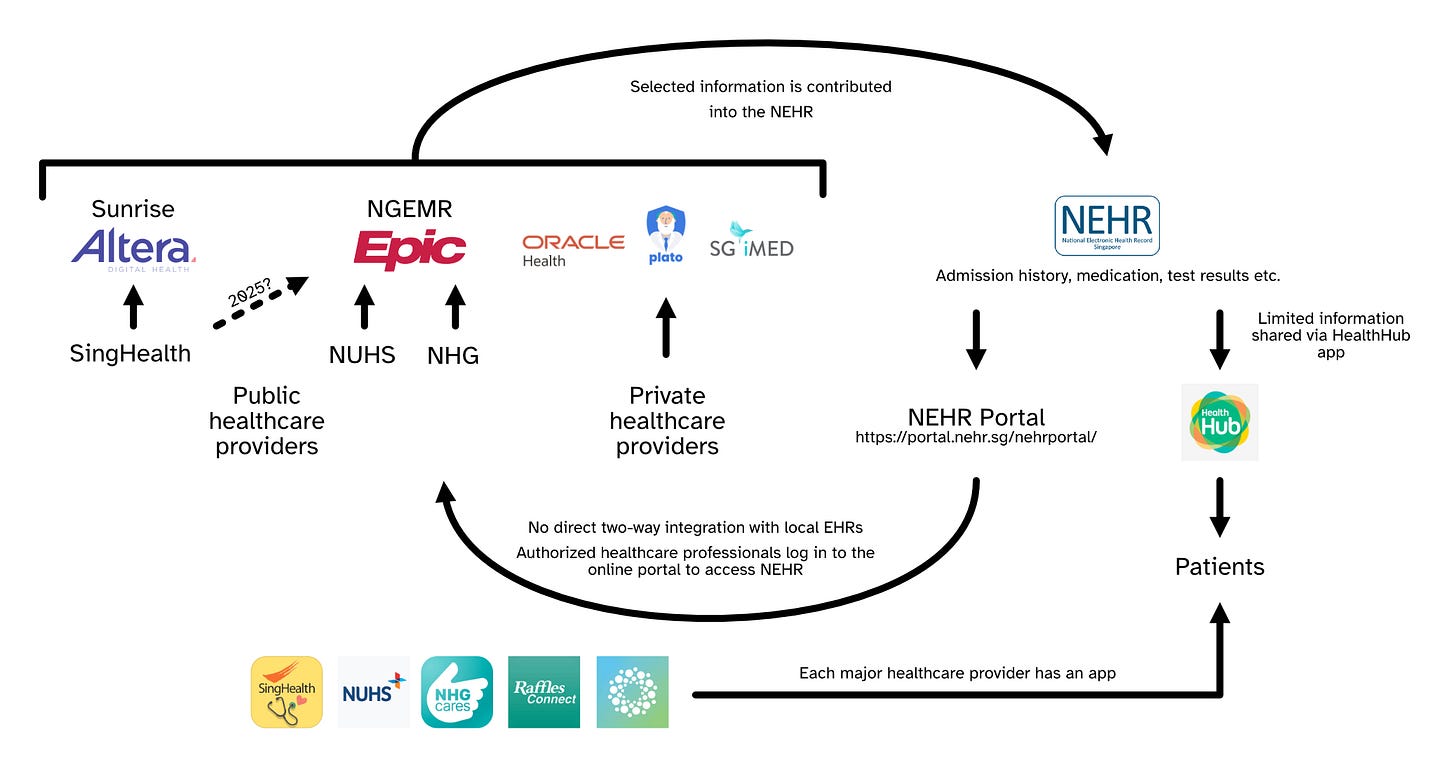
Singapore’s public healthcare is divided into three major clusters— SingHealth, National University Health System (NUHS), and National Health Group (NHG). SingHealth employs Sunrise by Altera Digital Health, while NHG and NUHS rely on the Next Generation Electronic Medical Record (NGEMR) powered by Epic Systems. This means doctors at SingHealth hospitals cannot access patient records in NHG and NUHS to understand their medical history, and vice versa. Thankfully, this is set to change with SingHealth’s migration to the NGEMR, likely in 2025.
Then we have the EHR systems used by private healthcare institutions. These include larger enterprise software like Oracle Cerner used by larger private groups like Raffles Medical Group and Parkway Pantai, as well as smaller SaaS solutions employed by smaller GP clinics and private specialists, such as Plato Medical and SGiMED.
Due to the different systems, information is largely siloed and disconnected between healthcare providers. And each EHR system has no incentive to share data with their competitors. Each major healthcare provider also has its own patient-facing app containing its slice of patient records. (Some data, such as blood tests and imaging results, does have partial integration between some providers, to facilitate broader diagnoses. That being said, despite all of the recent advancements, we did hear accounts of MRI scans still being delivered on CD-ROMs.)
But Singapore is taking active steps to resolve the data fragmentation via the National Electronic Health Record (NEHR). This national platform is accessible by all public hospitals and participating private providers and includes key information such as a patient’s medical history, prescribed medication, health checkups, vaccinations, and imaging results.
Admittedly, participation remains spotty in the private sector with only about 15% of private providers contributing. But an upcoming Health Information Bill that mandates all healthcare providers to contribute records to the NEHR could eventually pave the way for a truly unified database.
Why doctors hate their EHRs
Large enterprise EHR systems are often classic case studies of poor user experience, mainly due to buyer-user misalignment. Hospital administrators buying EHR software have different priorities from the healthcare professionals who rely on these systems everyday:
Administrator focus on liability concerns often manifest in the form of excess alerts, which cripples usability and creates alert fatigue
A focus on cost minimization often has disastrous consequences—bad localization, rushed implementations, and cheap but slow servers
A single one-size-fits-all solution can simplify procurement but also leads to a cluttered interface with too many features serving too many stakeholders
In our conversations with healthcare professionals, many public clinicians expressed varying levels of dissatisfaction with Epic, which seems to concur with reviews around the world.
For example, a $500 million implementation of Epic Systems in Denmark had a fundamental translation issue.
“C-section,” in the Danish version, referred to an executive suite, not an emergency birth procedure. The American specialty “speech and language pathologist” does not exist in Denmark. The Danish system for a short time offered surgeons the choice of amputating the left leg or the “correct” leg. Lost in translation: Epic goes to Denmark
And as mentioned at the beginning of this essay, the Europeans even went on strike because of Epic. In Norway, healthcare providers organized demonstrations against their Epic health platform and close to 90% of surveyed doctors at St. Olav's University Hospital believed that the platform was a threat to patient health.
Yet Epic is far from the only EHR software to face criticism.
In the early 2000s, the United States’ Department of Defense implemented AHLTA, a global EHR system for their facilities. Its Wikipedia article is relatable for anyone who has to interact with slow software everyday:
Current providers using AHLTA have become excellent at multi-tasking while using the application as it routinely takes 30sec-1min to load up each new tab that is requested. Armed Forces Health Longitudinal Technology Application
At the Children’s Hospital of Pittsburgh, the implementation of Oracle Cerner, the second largest EHR provider after Epic Systems, correlated with a doubling of mortality rates for an emergency patient population. And when the US Veterans Health Administration attempted to migrate from its previous system VistA to Cerner, there were numerous problems including 149 instances of patient harm, and a bill was officially issued to terminate the contract.
As Atul Gawande summarizes eloquently in a New Yorker article titled “Why Doctors Hate Their Computers”:
But three years later I’ve come to feel that a system that promised to increase my mastery over my work has, instead, increased my work’s mastery over me.
Beyond digital filing cabinets
When regular software fails its users, the worst outcomes are high churn rates and negative reviews. But when an EHR system fails, lives are literally at risk. To build a better EHR, we need to look beyond digital filing cabinets and realize that we are deploying fundamental infrastructure for modern healthcare. It is not about faster horses, but an entire automobile revolution.
We believe the next breakthrough EHR company will have to deliver on three fronts—proactive analytics, privacy-preserving interoperability, and a better user interface.
1. Proactive analytics
EHR systems contain a tremendous wealth of data that can do so much more. Imagine an EHR that automatically highlights potential adverse drug reactions based on a patient’s medical history or even genetics. How about EHR that suggests relevant screenings and tests and schedules them with a click of a button? Or an EHR that alerts healthcare providers about potential abuse of prescribed drugs?
These ideas seem obvious, and the technology is far from novel. But current implementations like Best Practice Advisories (BPAs) often fall short, overwhelming doctors with excessive notifications that are repetitive and irrelevant. In one study, researchers found that drug safety alerts were overridden as much as 96% of the time, due to false alarms, repeated alerts, and unclear messages.

In contrast, a Singapore study found that careful governance of which BPAs to show can dramatically reduce the number of irrelevant alerts and significantly increase meaningful remedial actions taken.
This highlights the importance of thoughtful design. Instead of overwhelming doctors with repetitive reminders, selectively present the most critical information. Instead of merely suggesting a screening, automatically schedule appointments with one click. Instead of calling out problematic drug interactions, suggest suitable alternatives.
Furthermore, such proactive features can also target patients directly, reminding them for relevant tests, flagging harmful prescription combinations, and providing real-time notifications if their vitals reach dangerous levels.
2. Privacy-preserving interoperability
When we asked local doctors about the prospects of an EHR that unifies patient data across private healthcare providers and public hospitals, a common retort is that it will never exist because of PDPA, Singapore’s equivalent of the GDPR. But does this really hold up? When a single patient’s data is fragmented across multiple providers, who are we really protecting?
Patient data, like financial data, is hypersensitive and very regulated. So why does financial data seem to flow so much more easily?
Perhaps public perceptions and regulations surrounding medical records are stricter than those around financial data. In that case, why not explore privacy-preserving interoperability? In my time at Google’s Payments Privacy Working Group, I had the privilege of looking into privacy technologies like differential privacy, homomorphic encryption, and federated learning. These are well-known techniques that allow data to be shared in a provably private manner. Leveraging these technologies, we could enable interoperability while fully respecting patient privacy:
Frameworks like Carequality, TEFCA, and CommonWell are setting standards for secure exchange of medical data and nationwide interoperability in the US
Products like Health Gorilla and Apple’s Health Records feature supports end-to-end encryption where Apple does not have access to encryption keys
Owkin collaborates with data providers to train AI models using federated learning, ensuring that data is never directly shared
During the COVID-19 pandemic, Google released the Community Mobility Reports, which aggregated patient statistics using anonymization technology including differential privacy
3. A better user experience
Healthcare software is far too important for a crappy user experience. Forcing healthcare professionals to struggle with frustrating interfaces puts the lives and well-being of vulnerable patients in real danger.
Earlier, we cited a study that demonstrated how careful governance of BPAs can significantly improve their effectiveness. It seems like a trivial solution: just put more effort into deciding which alerts to show. But the truth is that this entails a deep understanding of clinical workflows and the needs of healthcare providers.
This is a textbook exercise in UIUX development. It demands that software providers put their users front and center. It calls for deep empathy for the doctors that use this software everyday, and for the patients that they are saving.
Imagine an EHR that fits seamlessly into the workflow of a healthcare provider without requiring hours of training or extensive customization.
“Stop asking me what’s my name and today’s date.” - Automatically populate forms with known information, such as the physician's name or today’s date
“I can’t remember which sub-sub-sub-menu has the option I want.” - A universal search bar to quickly search and navigate across screens
“I have no time to wait for this to load.” - Instant latency and graceful degradation
“Remind me what does this mean again?” - Highlight terminology for contextual explanations
It should feel like an extension of the doctor’s hands and mind. Or better yet, fade invisibly into the background, letting healthcare professionals focus on diagnosing, treating, and healing. I suspect doing this well entails a holistic approach that goes beyond software. Every touchpoint—from the speed and reliability of the servers, to the usability of devices in a clinical setting—must be designed to support a frictionless experience.
The world needs the most user-friendly and compliant EHR system that anyone has ever seen—so good that doctors demand it and patients expect it.
Truly epic: a patient-centric EHR
Most advice on B2B and enterprise sales focuses on highlighting the business value of your solution. And because there are more parties involved in the sales process, stakeholder management becomes the primary concern.
But in healthcare, where the primary goal is saving lives, the common B2B advice misses the mark. An EHR cannot prioritize liability mitigation or cost cutting above the needs of doctors and their patients. The constant juggling of business objectives and complex stakeholder relationships ultimately corrupts the value of EHR systems and frustrates the very people they are meant to serve.
The only true measure of an EHR is how well it improves patient outcomes.
Since the B2B sales cycle is what breaks EHR, why not get rid of it and adopt a B2C approach directly targeting the end users? And since doctors have little control over the systems they use in hospitals, this leaves us with one critical stakeholder—the patients.
Imagine an EHR built for patients.
As a first prototype, we start with a patient-facing platform where users export and consolidate their medical data from different providers in one simple, intuitive interface. Patients can then share this data when engaging new healthcare providers, or with their caregivers for care coordination. The initial value proposition is interoperability—to unify and transfer data seamlessly for users navigating multiple different healthcare providers.
Early adopters could be frequent globetrotters with healthcare data spread across different countries, or patients with complex conditions that require interactions with many providers.
Subsequently, it can combine data from wearables, diet, exercise and other lifestyle attributes, allowing for a comprehensive view of their health that supports analytics and personalized recommendations and reminders. This can in turn assist doctors in providing better diagnosis and treatments.
We are already seeing early steps towards a patient-centric EHR, with efforts like Google Health’s initial foray in 2008, Apple Health’s Health Records launched in 2018, and offerings from companies like Guava Health and Picnic Health. Not all of these will succeed. But the shift towards a patient-centric EHR is more feasible than ever, thanks to recent regulatory changes that emphasize patient ownership of data and interoperability.
For example, the EU’s GDPR mandates the right to data portability, giving patients the right to export their personal data from healthcare providers. In the US, regulations and frameworks like the HIPAA, the 21st Century Cures Act, and TEFCA empower patients to access their medical records and transfer this data across providers and applications. New rules from CMS and HHS, finalized in 2024, aim to enforce interoperability of healthcare records and prevent information blocking, further supporting this shift.
In the long run, we believe a patient-centric model for EHR software could transform the dynamics of healthcare, elevating patients from passive recipients to active participants in their own treatment. In an age of value-based care, such a transformation could redefine the entire healthcare experience.
This would require a fundamental rethinking of how EHRs are built and sold, but it holds the potential to truly revolutionize the industry. After all, if the goal is better patient care, why not start by putting the EHR in the hands of the patient?